What is tenosynovial giant cell tumor (TGCT)?
TGCT is a disease where tumors form in the body's joints that cause pain, inflammation, and loss of function. While non‑cancerous, the disease can permanently damage the joint and surrounding tissue.
There are 11-50 cases of TGCT per million people annually.
92
%
of people with TGCT
experienced pain*
85
%
of people living with
TGCT
reported swelling*
*According to a survey of 497 patients with TGCT
What causes TGCT?
Research shows that TGCT forms when cells abnormally produce too much of a protein called colony stimulating factor 1 (CSF1), leading to tumor formation. This protein attracts immune cells expressing colony stimulating factor 1 receptor (CSF1R), leading to inflammation and potentially permanent joint damage.
PVNS? GCT‑TS?
It's all TGCT
TGCT used to be referred to as pigmented villonodular synovitis (PVNS) and giant cell tumor of the tendon sheath (GCT‑TS). In 2013, the World Health Organization reclassified GCT‑TS, PVNS and diffuse‑type giant cell tumor all as TGCT.
The various names can be confusing, but when in doubt, just remember PVNS and GCT‑TS are all the same disease: TGCT.
SEE GLOSSARY OF TERMS
Types of TGCT
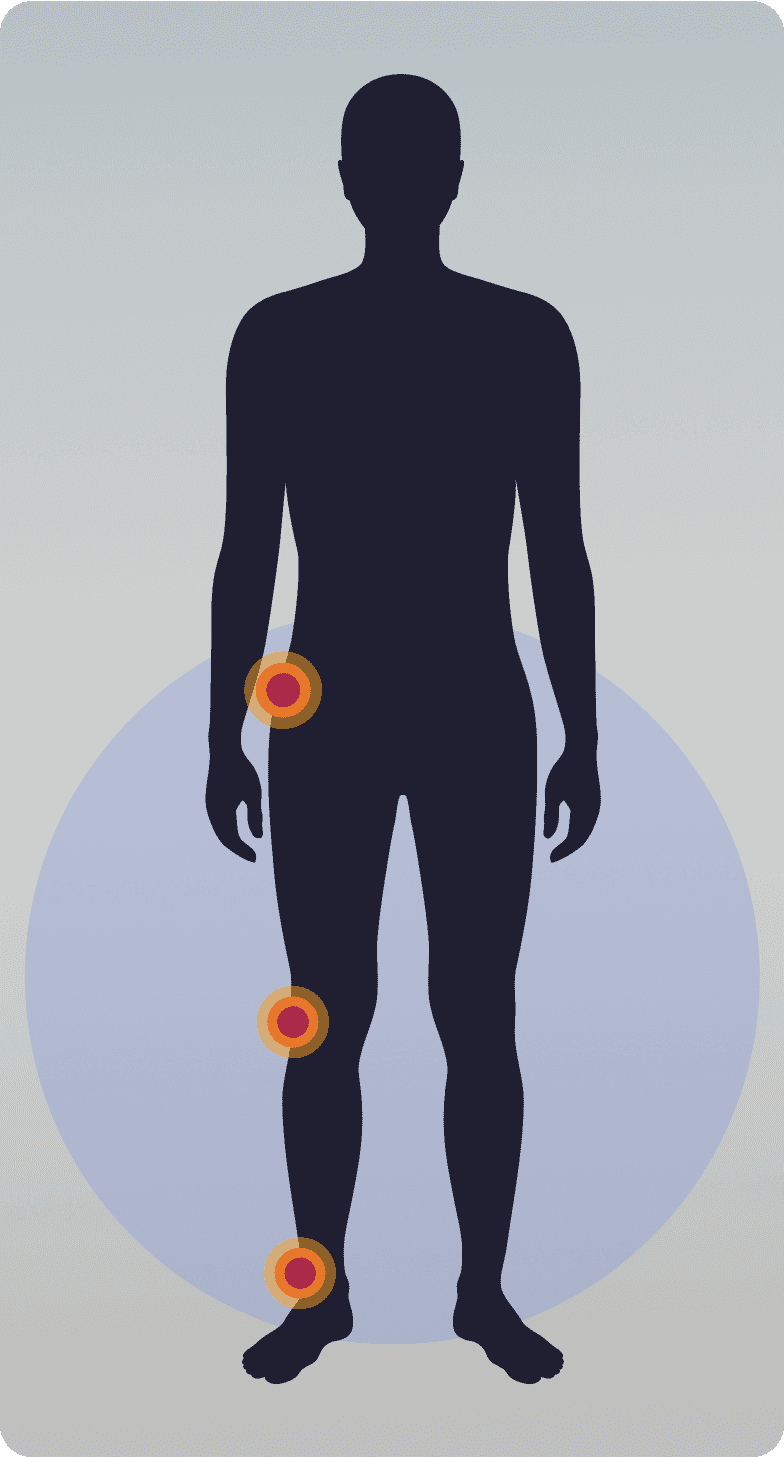
There are two types of TGCT: localized/nodular and diffuse. Localized/nodular TGCT tends to be smaller tumors inside of the joint, while diffuse TGCT tumors are larger, without distinct boundaries.
Your experience may be different from other patients, depending on your unique TGCT and tumor location.
Localized/nodular TGCT
More common
Lifetime recurrence rate: up to 15%
Usually single, well-defined tumor, usually nodular
Often does not cause pain or joint dysfunction
Tumor location:Tends to impact smaller joints like hands, fingers, wrist, feet
Diffuse TGCT
Less common
Lifetime recurrence rate: up to 72%
lll-defined tumors that invade the joint
Can extend out of the joint and damage surrounding bone
Tumor location:Tends to impact larger joints like knee, hip, ankle
In a survey of 289 people
living with TGCT,
72
%
of people with diffuse TGCT had
at least 1 recurrence after surgery
Symptoms
People with symptomatic TGCT often suffer from:
Pain
Swelling
Stiffness
Instability
Reduced range of motion
Diagnosis
Getting diagnosed with TGCT can be a journey in itself. Symptoms can mimic those of other diseases and not all doctors have experience with TGCT, which is why it's crucial to consult a doctor that has experience treating TGCT and can lead you to a multi‑disciplinary team of experts.
Find Your Care TeamIT CAN TAKE UP TO
3-4 YEARS
TO GET A TGCT DIAGNOSIS
There are multiple steps to a TGCT diagnosis, which Can include the following:
Physical exam
Full analysis of medical history
X-ray
MRI
CT scan
Biopsy
While there are various options for imaging, an MRI is recommended, followed by a biopsy. A definitive diagnosis of TGCT is normally obtained through a biopsy and will help you and your care team understand what treatment option may be best for your specific TGCT.
MRI=magnetic resonance imaging; CT=computerized tomography.